m (Unprotected "Somogyi rebound": Bot: Unprotecting page) |
|||
| (36 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
| − | '''Somogyi rebound''' aka "Somogyi's phenomenon" is a common phenomenon in pet diabetes : When blood sugar levels drop too far or too fast, the |
+ | '''Somogyi rebound''' aka "Somogyi's phenomenon" and rebound hyperglycemia,<ref name=ADA>{{cite web|url=http://diabetes.diabetesjournals.org/content/37/12/1608|title=Glucose counterregulation and its impact on diabetes mellitus|author=Gerich, J.E.|publisher=Diabetes (American Diabetes Association)|date=December 1988}}</ref> is a common phenomenon in pet diabetes : When blood sugar levels drop too far or too fast, the counterregulatory hormones which raise blood glucose are activated, causing stored glucose from the liver to enter the bloodstream, resulting in high blood sugar. |
==What you'll see== |
==What you'll see== |
||
| + | [[Image:DiabeteDiagram.jpg|thumb|right|300px|What can be seen in a curve. These overlays of hypothetical insulin curves show what's wrong or right with the blood glucose readings turned into a graph. The red line shows what Somogyi rebound looks like on a graphed curve-extreme lows and extreme highs.]] |
||
| ⚫ | It's confusing but true: Too little insulin means pre-shot blood tests are too high; too much insulin often also means pre-shots are too high. This effect is often noted by those who test their pets' blood glucose at home. It means that even when blood glucose levels are too high, simply raising insulin dosage can make things worse instead of better.<ref name=Feeney>{{cite web|url=http://images2.wikia.nocookie.net/diabetesindogs/images/6/61/CESA_September_07.pdf|title=How Do You Solve a Problem Like Diabetes?|author=Feeney, Clara|publisher=Irish Veterinary Journal|date=September 2007}} pages 2-3</ref> |
||
| ⚫ | If you can think of it in terms of bouncing a ball, the harder you throw the ball on the ground, the higher it bounces back up; throwing it down softer means it doesn't bounce back as high. Reducing the insulin dose would represent "throwing the ball on the ground softer", because it means the [[Counter-Regulatory hormones|counter-regulatory hormones]] aren't activated, causing the [[Blood glucose level|blood glucose levels]] to "bounce" back up. |
||
| ⚫ | It's confusing but true: Too little insulin means pre-shot blood tests are too high; too much insulin often also means pre-shots are too high. This effect is often noted by those who test their pets' blood glucose at home. It means that even when blood glucose levels are too high, simply raising insulin dosage can make things worse instead of better. |
||
| ⚫ | If you are testing urine for glucose, you may also see [[glycosuria]] (glucose in the urine) within a 24 hour period when there's Somogyi. <ref>{{cite web|url=http://www.noahcompendium.co.uk/Intervet_Schering-Plough/Caninsulin___Suspension_for_injection/-28708.html |publisher=NOAH Compendium-UK|title=Caninsulin-General}}</ref> Just as with high blood glucose levels during Somogyi, raising the dose of insulin will only make the problem worse. |
||
| ⚫ | If you can think of it in terms of bouncing a ball, the harder you throw the ball on the ground, the higher it bounces back up; throwing it down softer means it doesn't bounce back as high. Reducing the insulin dose would |
||
| ⚫ | It's not always easy to tell a rebound from a regular curve showing insulin action ending normally. One way to tell the difference is to take a [[curve]] (repeated tests every 2 hours starting with the insulin shot) and look for the shape of the curve. If the curve is valley-shaped, and gradual, then you are not seeing Somogyi rebound. Other shapes should arouse suspicion. In particular, if the rise after peak action is faster and rises higher than the original pre-insulin level and the original fall in blood sugar, you have good cause to consider rebound. The only sure way to check is to reduce dosage and look for a better-shaped curve. |
||
| ⚫ | If you are testing urine for glucose, you may also see [[glycosuria]] (glucose in the urine) within a 24 hour period when there's Somogyi<ref> |
||
| + | |||
| ⚫ | |||
==What's going on== |
==What's going on== |
||
| − | The reason: Anytime the glucose level drops too far or too fast, the |
+ | The reason: Anytime the glucose level drops too far or too fast, the body's defense mechanisms are triggered, releasing [[Counterregulatory hormones|hormones]] epinephrine and cortisol, [[Counterregulatory hormones|growth hormone]] and [[glucagon]] <ref>{{cite web|url=http://web.archive.org/web/20061104180550/http://www.caninsulin.com/documents/061626.pdf |title=Caninsulin-Somogyi Effect-Page 4|publisher=Intervet}}</ref> into the bloodstream, causing temporary insulin-resistance. These hormones in turn cause [[glycogenolysis|glucose]] to be released into the blood by breaking down glycogen from the liver and the result is [[hyperglycemia]].<ref>{{cite web|url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=Abstract&list_uids=6387483&query_hl=1&itool=pubmed_DocSum |title=Glucose Counterregulation & Insulin Waning in Somogyi Phenomenon|publisher=New England Journal of Medicine|year=1984|author=Bolli GB, Gottesman IS, Campbell PJ, Haymond MW, Cryer PE, Gerich JE.}}</ref> If these are insufficient, [[hypoglycemia]] ensues.<ref>{{cite web|url=http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/pancreas/glucagon.html |publisher=Colorado State University School of Veterinary Medicine|title=Glucagon}}</ref> |
| − | Even when raising the insulin dose slowly and carefully, it's possible to pass the correct dose and go on to an overdose. |
+ | Even when raising the insulin dose slowly and carefully, it's possible to pass the correct dose and go on to an overdose. This may produce a rebound -- a swift jump in blood glucose up from a dangerously low reading, to beyond the previous pre-shot level. The pet may be a bit less responsive to the same dose the next shot. Repeating the overdose on subsequent days, and checking only pre-shot readings or urine glucose, can give the dangerously wrong impression that more insulin is needed! Remember to check occasionally at the expected nadir (low point) as well. |
| − | The effect is probably underrecognized in humans, as many also suffer the same ill effects from rapid or steep blood glucose drops<ref> |
+ | The effect is probably underrecognized in humans, as many also suffer the same ill effects from rapid or steep blood glucose drops. <ref> {{cite web|url=http://web.archive.org/web/20060704041155/http://www.umassmed.edu/diabeteshandbook/chap08.htm |publisher=University of Massachusetts|title= Diabetes Handbook-Questions & Answers}}</ref> This postgraduate medicine article regarding treatment of diabetes in people refers to Somogyi as "repetitive rebound hypoglycemia", calling it an easily treatable factor of poor control. <ref>{{cite web|url=http://web.archive.org/web/20080122035318/http://www.postgradmed.com/issues/2002/05_02/stoller2.htm |publisher=Postgradmed.com|year=2002|title=Individualizing Insulin Management}}</ref> It was first documented by a Dr. Somogyi in 1938 <ref>{{cite web|url=http://www.whonamedit.com/synd.cfm/2067.html |publisher=Whonamedit.com|title=Somogyi's Phenomenon}}</ref> as "[[Hypoglycemia]]-induced [[Hyperglycemia]]".<ref>{{cite web|url=http://www.emedicine.com/med/topic2098.htm |publisher=eMedicine-WebMD|title=Somogyi Phenomenon}}</ref><ref>{{cite web|url=http://www.indulgedfurries.com/petdiabetes/somogyi.htm |publisher=Petdiabetes.org|title=Somogyi Rebound}}</ref> |
| − | A good explanation of Somogyi is that it occurs when too much insulin has been administered, '''but''' the amount of overdose is '''not''' enough to cause an '''actual, full-blown''' [[hypoglycemia]] incident. Because the body detects the fall in blood glucose, the [[counterregulatory hormones]]<ref> |
+ | A good explanation of Somogyi is that it occurs when too much insulin has been administered, '''but''' the amount of overdose is '''not''' enough to cause an '''actual, full-blown''' [[hypoglycemia]] incident. Because the body detects the fall in blood glucose, the [[counterregulatory hormones]]. <ref>{{cite web|url=http://www.aapsj.org/abstracts/AM_2008/AAPS2008-001530.PDF |title=Cortisol Response to Hypoglycemia|publisher=AAPSJ|author=Lim, CN, et. al.}} </ref> are released just as though it was a true hypo emergency. They signal the liver to release its [[glycogen]] stores and convert it back to glucose. <ref>{{cite web|url=http://www.noahcompendium.co.uk/Intervet_Schering-Plough/Caninsulin___Suspension_for_injection/-28708.html |publisher=NOAH Compendium-UK|title=Caninsulin-General}}</ref> |
==What if you don't stop it?== |
==What if you don't stop it?== |
||
| − | [[Image:Somogyi. |
+ | [[Image:Somogyi.JPG|thumb|350px|right|Somogyi rebound-a theoretical graph of what happens if you ignore the low bg numbers and focus only on the high ones created by the lows. As the insulin dose increases, the lows become lower, causing the counter-regulatory hormones to send the bg's higher in response. The only way to stop the extreme highs is to stop the lows; this means LESS insulin rather than more because it is the lows which are responsible for creating the highs <ref>{{cite web|url=http://en.wikipedia.org/wiki/Chronic_Somogyi_rebound#Background|publisher= Wikipedia|title=Somogyi Rebound}}</ref>.]] It's unusual to be monitoring glucose right when this happens, and typical to just continue the overdose, leading to a repeated rebound situation. So it's good to learn to recognize the patterns of repeated rebound. |
| − | * A typical rebound pattern, most often seen with long-acting insulins, is a '''high, flat, unresponsive blood sugar''' |
+ | * A typical rebound pattern, most often seen with long-acting insulins, is a '''high, flat, unresponsive blood sugar'''. This high flat curve will be punctuated by sudden drops to very low values, (with possible hypoglycemic events) followed by a fast return to high unresponsive numbers. (It's the sudden dip that distinguishes this pattern from inadequate insulin.) |
* When using shorter-acting insulins, repeated Somogyi rebound may manifest instead as '''rapidly alternating high and low blood sugar''' numbers with no apparent logic. The highs and lows will both be exaggerated compared to what you'd see on a smaller dose. |
* When using shorter-acting insulins, repeated Somogyi rebound may manifest instead as '''rapidly alternating high and low blood sugar''' numbers with no apparent logic. The highs and lows will both be exaggerated compared to what you'd see on a smaller dose. |
||
| ⚫ | |||
==When to suspect this== |
==When to suspect this== |
||
| ⚫ | Any time blood glucose numbers seem <i>higher</i> after dosage is raised, consider the possibility of a somogyi rebound .<ref>{{cite web|url=http://en.wikipedia.org/wiki/Chronic_Somogyi_rebound#Detection|publisher= Wikipedia|title=Somogyi Rebound Detection}}</ref> But other things can cause unexpectedly high blood glucose too, so look for a clear correlation with dosage changes. |
||
| ⚫ | It's not always easy to tell a rebound from a regular curve showing insulin action ending normally. One way to tell the difference is to take a [[curve]] (repeated tests every 2 hours starting with the insulin shot) and look for the shape of the curve. If the curve is valley-shaped, and gradual, then you are not seeing Somogyi rebound. Other shapes should arouse suspicion. In particular, if the rise after peak action is faster and rises higher than the original pre-insulin level and the original fall in blood sugar, you have good cause to consider rebound. The only sure way to check is to reduce dosage and look for a better-shaped curve. |
||
| − | |||
| ⚫ | |||
'''[[Glycogenolysis]]''': The liver may dump glucose in reponse to other events, too. See also [[Regulation difficulties]]. |
'''[[Glycogenolysis]]''': The liver may dump glucose in reponse to other events, too. See also [[Regulation difficulties]]. |
||
| Line 42: | Line 43: | ||
|style="height:1px;border:0;" colspan="3"| |
|style="height:1px;border:0;" colspan="3"| |
||
|-valign="top" |
|-valign="top" |
||
| − | |style="padding:5px;border:2px solid #ffb6c1;background-color:#ffe4e1;" width=" |
+ | |style="padding:5px;border:2px solid #ffb6c1;background-color:#ffe4e1;" width="100%"| |
| − | Rebound is a vicious circle, with the body going either at or near [[hypoglycemia]] from the effects of too much insulin. |
+ | Rebound is a vicious circle, with the body going either at or near [[hypoglycemia]] from the effects of too much insulin.<ref name=Feeney/> |
When the lows occur, the body's "self-defense" mechanisms set to work, producing hormones which are meant to raise blood glucose levels. Of course they do, and the result is [[hyperglycemia]]. The systems of living beings do very little abruptly; it's more of an easing into or easing out of a situation or condition. |
When the lows occur, the body's "self-defense" mechanisms set to work, producing hormones which are meant to raise blood glucose levels. Of course they do, and the result is [[hyperglycemia]]. The systems of living beings do very little abruptly; it's more of an easing into or easing out of a situation or condition. |
||
| − | It may take a few days after the insulin dose has been adjusted downward for the [[hyperglycemia|high blood glucose]] which follows [[hypoglycemia]] to return to normal<ref> |
+ | It may take a few days after the insulin dose has been adjusted downward for the [[hyperglycemia|high blood glucose]] which follows [[hypoglycemia]] to return to normal. <ref>{{cite web|url=http://www.vetsulin.com/PDF/20585.pdf |title=Vetsulin-Somogyi Effect (Page 21)|publisher=Intervet}}</ref><ref name=Feeney/> |
| − | Just '''one''' at or near [[hypoglycemia]] incident can release [[cortisol]] into the blood, which can keep blood glucose values elevated for up to 3 days. |
+ | Just '''one''' at or near [[hypoglycemia]] incident can release [[cortisol]] into the blood, which can keep blood glucose values elevated for up to 3 days.<ref name=Feeney/> |
| − | When non-diabetics have [[hypoglycemia|hypoglycemic]] episodes from things like crash diets, skipping meals, etc., they also have rebound hyperglycemia from them, but they don't end up with Somogyi. The difference is that the pancreas of the non-diabetic is able to secrete enough insulin to negate the surge in blood glucose, and continue producing enough insulin to keep it down<ref> |
+ | When non-diabetics have [[hypoglycemia|hypoglycemic]] episodes from things like crash diets, skipping meals, etc., they also have rebound hyperglycemia from them, but they don't end up with Somogyi. The difference is that the pancreas of the non-diabetic is able to secrete enough insulin to negate the surge in blood glucose, and continue producing enough insulin to keep it down. <ref>{{cite web|url=http://www.vetsulin.com/PDF/20585.pdf |title=Vetsulin-Somogyi Effect (Page 21)|publisher=Intervet}}</ref> |
Those with diabetes must depend on their insulin injections to do this for them; giving more insulin in response to the rebound [[hyperglycemia]] only establishes or re-establishes the Somogyi pattern. |
Those with diabetes must depend on their insulin injections to do this for them; giving more insulin in response to the rebound [[hyperglycemia]] only establishes or re-establishes the Somogyi pattern. |
||
|} |
|} |
||
| − | |||
| ⚫ | |||
| − | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| − | *[http://www.petalk.com/feline-diabetes.html A Good-Talk-You-Through Page for Somogyi and Pets-PetTalk] |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
==References== |
==References== |
||
| Line 73: | Line 62: | ||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| + | [[Category:Conditions]] |
||
| + | [[Category:Terms]] |
||
| ⚫ | |||
| + | [[Category:Content]] |
||
Latest revision as of 23:22, 23 May 2012
Somogyi rebound aka "Somogyi's phenomenon" and rebound hyperglycemia,[1] is a common phenomenon in pet diabetes : When blood sugar levels drop too far or too fast, the counterregulatory hormones which raise blood glucose are activated, causing stored glucose from the liver to enter the bloodstream, resulting in high blood sugar.
What you'll see[]
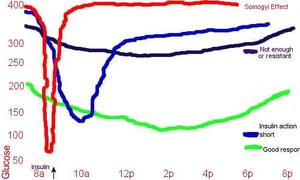
What can be seen in a curve. These overlays of hypothetical insulin curves show what's wrong or right with the blood glucose readings turned into a graph. The red line shows what Somogyi rebound looks like on a graphed curve-extreme lows and extreme highs.
It's confusing but true: Too little insulin means pre-shot blood tests are too high; too much insulin often also means pre-shots are too high. This effect is often noted by those who test their pets' blood glucose at home. It means that even when blood glucose levels are too high, simply raising insulin dosage can make things worse instead of better.[2]
If you can think of it in terms of bouncing a ball, the harder you throw the ball on the ground, the higher it bounces back up; throwing it down softer means it doesn't bounce back as high. Reducing the insulin dose would represent "throwing the ball on the ground softer", because it means the counter-regulatory hormones aren't activated, causing the blood glucose levels to "bounce" back up.
If you are testing urine for glucose, you may also see glycosuria (glucose in the urine) within a 24 hour period when there's Somogyi. [3] Just as with high blood glucose levels during Somogyi, raising the dose of insulin will only make the problem worse.
It's not always easy to tell a rebound from a regular curve showing insulin action ending normally. One way to tell the difference is to take a curve (repeated tests every 2 hours starting with the insulin shot) and look for the shape of the curve. If the curve is valley-shaped, and gradual, then you are not seeing Somogyi rebound. Other shapes should arouse suspicion. In particular, if the rise after peak action is faster and rises higher than the original pre-insulin level and the original fall in blood sugar, you have good cause to consider rebound. The only sure way to check is to reduce dosage and look for a better-shaped curve.
What's going on[]
The reason: Anytime the glucose level drops too far or too fast, the body's defense mechanisms are triggered, releasing hormones epinephrine and cortisol, growth hormone and glucagon [4] into the bloodstream, causing temporary insulin-resistance. These hormones in turn cause glucose to be released into the blood by breaking down glycogen from the liver and the result is hyperglycemia.[5] If these are insufficient, hypoglycemia ensues.[6]
Even when raising the insulin dose slowly and carefully, it's possible to pass the correct dose and go on to an overdose. This may produce a rebound -- a swift jump in blood glucose up from a dangerously low reading, to beyond the previous pre-shot level. The pet may be a bit less responsive to the same dose the next shot. Repeating the overdose on subsequent days, and checking only pre-shot readings or urine glucose, can give the dangerously wrong impression that more insulin is needed! Remember to check occasionally at the expected nadir (low point) as well.
The effect is probably underrecognized in humans, as many also suffer the same ill effects from rapid or steep blood glucose drops. [7] This postgraduate medicine article regarding treatment of diabetes in people refers to Somogyi as "repetitive rebound hypoglycemia", calling it an easily treatable factor of poor control. [8] It was first documented by a Dr. Somogyi in 1938 [9] as "Hypoglycemia-induced Hyperglycemia".[10][11]
A good explanation of Somogyi is that it occurs when too much insulin has been administered, but the amount of overdose is not enough to cause an actual, full-blown hypoglycemia incident. Because the body detects the fall in blood glucose, the counterregulatory hormones. [12] are released just as though it was a true hypo emergency. They signal the liver to release its glycogen stores and convert it back to glucose. [13]
What if you don't stop it?[]
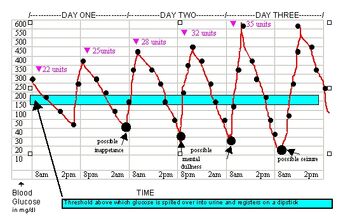
Somogyi rebound-a theoretical graph of what happens if you ignore the low bg numbers and focus only on the high ones created by the lows. As the insulin dose increases, the lows become lower, causing the counter-regulatory hormones to send the bg's higher in response. The only way to stop the extreme highs is to stop the lows; this means LESS insulin rather than more because it is the lows which are responsible for creating the highs [14].
It's unusual to be monitoring glucose right when this happens, and typical to just continue the overdose, leading to a repeated rebound situation. So it's good to learn to recognize the patterns of repeated rebound.
- A typical rebound pattern, most often seen with long-acting insulins, is a high, flat, unresponsive blood sugar. This high flat curve will be punctuated by sudden drops to very low values, (with possible hypoglycemic events) followed by a fast return to high unresponsive numbers. (It's the sudden dip that distinguishes this pattern from inadequate insulin.)
- When using shorter-acting insulins, repeated Somogyi rebound may manifest instead as rapidly alternating high and low blood sugar numbers with no apparent logic. The highs and lows will both be exaggerated compared to what you'd see on a smaller dose.
When to suspect this[]
Any time blood glucose numbers seem higher after dosage is raised, consider the possibility of a somogyi rebound .[15] But other things can cause unexpectedly high blood glucose too, so look for a clear correlation with dosage changes.
Glycogenolysis: The liver may dump glucose in reponse to other events, too. See also Regulation difficulties.
Insulin resistance in the case where raising dose appears to have no effect over a wide range of dosage, it can be difficult to distinguish Somogyi rebound from true Insulin resistance.
I've Lowered The Insulin Dose--Why Are My Pet's BG's Still High?[]
|
Rebound is a vicious circle, with the body going either at or near hypoglycemia from the effects of too much insulin.[2] When the lows occur, the body's "self-defense" mechanisms set to work, producing hormones which are meant to raise blood glucose levels. Of course they do, and the result is hyperglycemia. The systems of living beings do very little abruptly; it's more of an easing into or easing out of a situation or condition. It may take a few days after the insulin dose has been adjusted downward for the high blood glucose which follows hypoglycemia to return to normal. [16][2] Just one at or near hypoglycemia incident can release cortisol into the blood, which can keep blood glucose values elevated for up to 3 days.[2] When non-diabetics have hypoglycemic episodes from things like crash diets, skipping meals, etc., they also have rebound hyperglycemia from them, but they don't end up with Somogyi. The difference is that the pancreas of the non-diabetic is able to secrete enough insulin to negate the surge in blood glucose, and continue producing enough insulin to keep it down. [17] Those with diabetes must depend on their insulin injections to do this for them; giving more insulin in response to the rebound hyperglycemia only establishes or re-establishes the Somogyi pattern. | ||
References[]
- ↑ Gerich, J.E. (December 1988). Glucose counterregulation and its impact on diabetes mellitus. Diabetes (American Diabetes Association).
- ↑ 2.0 2.1 2.2 2.3 Feeney, Clara (September 2007). How Do You Solve a Problem Like Diabetes?. Irish Veterinary Journal. pages 2-3
- ↑ Caninsulin-General. NOAH Compendium-UK.
- ↑ Caninsulin-Somogyi Effect-Page 4. Intervet.
- ↑ Bolli GB, Gottesman IS, Campbell PJ, Haymond MW, Cryer PE, Gerich JE. (1984). Glucose Counterregulation & Insulin Waning in Somogyi Phenomenon. New England Journal of Medicine.
- ↑ Glucagon. Colorado State University School of Veterinary Medicine.
- ↑ Diabetes Handbook-Questions & Answers. University of Massachusetts.
- ↑ Individualizing Insulin Management. Postgradmed.com (2002).
- ↑ Somogyi's Phenomenon. Whonamedit.com.
- ↑ Somogyi Phenomenon. eMedicine-WebMD.
- ↑ Somogyi Rebound. Petdiabetes.org.
- ↑ Lim, CN, et. al.. Cortisol Response to Hypoglycemia. AAPSJ.
- ↑ Caninsulin-General. NOAH Compendium-UK.
- ↑ Somogyi Rebound. Wikipedia.
- ↑ Somogyi Rebound Detection. Wikipedia.
- ↑ Vetsulin-Somogyi Effect (Page 21). Intervet.
- ↑ Vetsulin-Somogyi Effect (Page 21). Intervet.
More Information[]
- Insulin-Induced Hyperglycemia in Dogs Nelson, Richard, et. al., 1982, Journal-American Veterinary Medical Association
- Somogyi explained Petdiabetes.org
- Somogyi Explained Auburn University
- Mini-Biography, Michael Somogyi
- Insulin vs. Glucagon Colorado State University College of Veterinary Medicine
- A Good-Talk-You-Through Page for Somogyi and Pets Rickards, Rick, PetTalk
The advice here re: adjusting insulin is very much like that given to people with diabetes in helping them manage their own insulin needs. - Hormones Which Raise or Lower Blood Glucose Clinical Chemistry
- Somogyi Effect Diabetes Self-Management