Injecting insulin at home is done subcutaneously, under the skin, but not into muscle or vein. See also Syringe and Insulin pen.
How to inject subcutaneously[]

Close-up illustration of a syringe needle showing bevel, point and heel.
It's best to pull up some loose skin into a tent then insert the needle firmly, bevel side up [1] for comfort.
BD has animations with narrations to help you learn how to draw insulin properly [2]. One can select from drawing one insulin or combining two insulins in the same syringe. Selecting this and the style of syringe you use personalizes the demo for your needs. The presentation is very clear and unhurried.
BD also has a slideshow which shows how to inject your dog. [3]

Correct way to give an injection when "tenting" the skin. This makes sure the insulin is injected into the skin flap created by "tenting" it. When the skin "tent" is released, the injected insulin is under it, or subcutaneous.
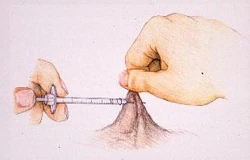
Wrong way to give a shot: The needle has totally passed through the "tented skin". The insulin, or any other injected drug, will be injected into the air. Note that in this graphic, the injection point is much closer to the "pinch" area holding the "tent" up. In the correct graphic, the injection point is closer to the body.
Injection tips[]
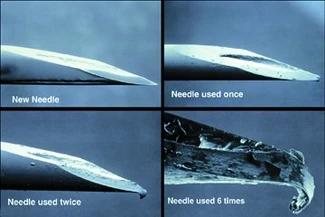
Better view of the needle bevel. See how it's angled to glide under the skin. If you look carefully, you can also see that the point of the needle begins to blunt after first use.
- Do NOT wipe the needle with alcohol as it removes the protective coating. The coating makes injection easier and less painful. [4]
- Injecting any insulin at the same site repeatedly over time or blunting a needle with re-use [5] can cause a lipodystrophy: either lipoatrophy [6] or lipohypertrophy. Either makes absorption unreliable. But varying the injection site can cause variability in action profile, too. This page illustrates [7] the most common areas humans with diabetes inject insulin and explains how absorption differs in various areas of the human body. This is true for ALL insulins. The new shot area needn't be very far from where the last shot was given--the distance of the width of 2 fingers will do fine as a measure. [8]. Most of us dealing with pet diabetes vary the side we give the injections in--right side mornings and left side evenings, for example. This is another help in avoiding giving shots in the same areas. [9][10]
- Many people give insulin shots in the scruff of the pet's neck, which is now considered to be a less than optimum choice. The neck area provides poor insulin absorption, due to it not having many capillaries, veins. etc. (vascularization).[11] Other sites suggested by Dr. Greco include the flank and armpit. [12] Intervet recommends giving injections from just back of the shoulder blades to just in front of the hipbone on either side, from 1 to 2 inches from the middle of the back. [13][10]

Note how the vial is held while drawing the insulin--at a slight angle, tilted so that the air space in the vial is at the opposite side the needle is drawing the insulin from; this helps reduce the possibility of bubbles in the syringe.
- To eliminate bubbles: If drawing insulin from a vial, set the syringe plunger to the dosage you want to draw, put the needle into the top of the vial while the vial is still upright, and push all the air out of the syringe. This will maintain air pressure equilibrium in the vial once you draw the dose and, because the vial is upright, will not cause air bubbles to mix with the solution. Turn the vial upside down and draw the insulin slowly.
- If you do get air bubbles into the syringe, it's ok with most insulins to re-inject the insulin into the vial and draw again until the air is gone. [14] Check that this is ok with your insulin. See also injecting insulin. Slower draw is less likely to draw bubbles.
- Some people prefer to gently jiggle their vials to make any air bubbles rise to the top, away from where the needle will draw.
|
From WebMD: [17] "If you notice an air bubble inside the syringe, draw a little extra insulin into the tube. Then, remove the needle from the bottle and hold the syringe-needle apparatus with the needle pointing toward the ceiling. Tap or flick the insulin syringe until the air bubble rises, and then push the plunger to force the air out of the syringe and get rid of any extra insulin." | ||
|
Some tips from Ed Bryant at National Federation for the Blind, who draws his own insulin. Quote: "How to Get Air Bubbles Out of an Insulin Syringe: [18] "There are techniques by which a blind diabetic may draw and mix insulin without drawing air into the syringe. Like many others, I have used them successfully for years. I first draw four or five units of regular insulin into the syringe and then inject all of it back into the vial. I then repeat the operation two more times. The fourth time, I draw the full amount of insulin needed from the first vial. Then, when I draw insulin from the second vial, I draw the exact amount needed. I have put this to the test; 100 repetitions without air bubbles. Diabetes Action Network former First Vice President Janet Lee twice performed the same test. In both cases the complete absence of air in the syringe was independently verified." | ||
- If you should bend a needle while drawing insulin, discard the syringe and start again; don't try to straighten it out. [14] Inserting the needle all the way into the vial makes it less easy to bend. [19]
Insulin tips[]
Cold insulin[]
Cold insulin [20] can sting, regardless of what species, type or brand. Bringing the insulin to room temperature by removing it from the fridge before actually using it can help avoid painful injections. Warming the capped insulin syringe with your hands can have the same effect. [21] Some people tuck the capped and filled syringe under their arm for a few minutes to warm it before use. Do NOT attempt to warm insulin using a stove, microwave, etc.; you may destroy the insulin by doing so. [4]
Don't Rub Injection Site![]
Rubbing the site where you gave the shot increases insulin absorption. [22] This means that the insulin is used faster than normal (no rubbing of the site) and might lead to a hypo. Rubbing the site increases blood flow to the area and this in turn speeds up absorption. [23][24][10]
Vary Injection Site[]
Placement of insulin injections can make a big difference. Absorption problems can occur possibly causing hypoglycemia [25] or hyperglycemia if the insulin injection sites are not varied. [26][10]
The area needn't be very far from where the last shot was given--the distance of the width of 2 fingers will do fine as a measure. [27]
When shots are given again & again into an area of skin, the tissue becomes thicker at that point; a fairly good analogy would be the calluses people get on hands and feet. The callus skin is thicker and harder; injection areas become similar to this too from repeated shots. This thicker, harder skin doesn't let the body absorb the injected insulin as well as thinner, non-hardened areas. [28][10]
Most of us dealing with pet diabetes vary the side we give the injections in--right side mornings and left side evenings, for example. This is another help in avoiding giving shots in the same areas.
Many people give insulin shots in the scruff of the pet's neck, which is now considered to be a less than optimum choice. The neck area provides poor insulin absorption, due to it not having many capillaries, veins. etc. (vascularization).
- Other sites suggested by Dr. Greco include the flank and armpit. [12]
- Intervet recommends giving injections from just back of the shoulder blades to just in front of the hipbone on either side, from 1 to 2 inches from the middle of the back [29].
Do not use the insulin if[]
Before each use, take a moment to inspect the insulin prior to drawing it into the syringe; clear insulins should appear not discolored and clear; suspended insulins should be uniform in their cloudiness. [30]
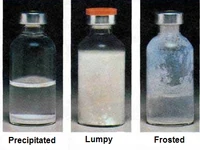
Three visual examples of damaged insulin.
|
Do not use the insulin if:
See Insulin problems for more information about "bad" insulin. | ||
Injection problems[]
There are sometimes leakage problems, when some insulin is lost when the needle is removed from the skin. [37] Some possible reasons and "fixes" for this are holding the "pinch" or "squeeze" too long which you made to give the shot.
The skin, now with insulin under it, is still being "squeezed" as it was before the insulin went under the skin. The "pinch" forces some of the insulin back out from the newly-created hole in the skin.
Releasing the "squeeze" or "pinch" first, then counting to 10 before removing the needle from the skin may give the insulin time to penetrate the fat layer and prevent leakage. Short needles can also cause insulin leakage--switching to longer ones can also help. [38]
See also diluting insulin, combining insulin, rolling insulin, syringes, Insulin use tips and Insulin pens. ![]()
References[]
- ↑ Subcutaneous Injection Page 4. Sarasota Memorial Hospital.
- ↑ Drawing Insulin Animation with Narration. BD Diabetes.
- ↑ Slideshow-Injecting a Dog. BD Diabetes.
- ↑ 4.0 4.1 Tips for Comfortable Injections. PetDiabetes.org. Cite error: Invalid
<ref>tag; name "PetDiabetes" defined multiple times with different content - ↑ Hanas, Ragnar. Insulin-Dependent Diabetes-page 21. Children With Diabetes.
- ↑ Hussein, Saleh Farag, Coates, Phillip, Green, Gill, Siddique, Haron (2006). Lipoatrophy can Happen With Any Subcutaneous Insulin. Endocrine Abstracts.
- ↑ Common Human Insulin Injection Areas & Their Absorption Rates. BD Diabetes.
- ↑ Tips for Injecting Insulin. Joslyn Diabetes Center.
- ↑ Greco, Deborah. FAQ's About Diabetic Dogs. BD Diabetes.
- ↑ 10.0 10.1 10.2 10.3 10.4 Heinemann, Lutz (January 2008). Variability of Insulin Action:Does It Matter?-page 40 (4 of 9). Insulin Journal. Cite error: Invalid
<ref>tag; name "Heinemann" defined multiple times with different content Cite error: Invalid<ref>tag; name "Heinemann" defined multiple times with different content Cite error: Invalid<ref>tag; name "Heinemann" defined multiple times with different content Cite error: Invalid<ref>tag; name "Heinemann" defined multiple times with different content - ↑ Greco, Deborah (2010). Treating Diabetes Mellitus in Dogs and Cats. Western Veterinary Conference.
- ↑ 12.0 12.1 Better Medicine E-Newsletter. Intervet (June 2006). Cite error: Invalid
<ref>tag; name "Intervet" defined multiple times with different content - ↑ Preparing Insulin & Giving Injection-Page 2. Intervet.
- ↑ 14.0 14.1 14.2 Injecting Insulin-Transcript of American Diabetes Association Videotape. American Diabetes Association (2003). Cite error: Invalid
<ref>tag; name "Videotape" defined multiple times with different content - ↑ How to Get Bubbles Out of Vetsulin (or any insulin). eHow.
- ↑ Insulin Administration-Position Statement. American Diabetes Association (2002).
- ↑ Giving A Dog Insulin #7. WebMD.
- ↑ Bryant, Ed. Blind Diabetes Can Draw Insulin Safely. National Federation for the Blind.
- ↑ Diabetes Mellitus. Washington State University.
- ↑ Injecting Cold Insulin. Diabetes Journals.
- ↑ Rickards, Rick. Tips and Tricks from Pet Owners. Pet Talk.com.
- ↑ Insulin Treatment-Factors Affecting Insulin Action. Patients Up To Date.
- ↑ Hirsch, Irl B. (2002). Insulin in the Hospital Setting-page 8. U of Washington Medical Center.
- ↑ Hanas, Ragnar. Insulin Dependent Diabetes in Children, Adolescents and Adults-Page 11-Factors Influencing the Insulin Effect. Children With Diabetes.
- ↑ Insulin-Section 6.1-Kinetics. InChem.
- ↑ Cook, Audrey (1 April 2010). Identifying the reasons behind difficult-to-control diabetes in dogs. DVM 360.
- ↑ Tips for Injecting Insulin. Joslyn Diabetes Center-Tips.
- ↑ Injection Site Selection. BD Diabetes.
- ↑ Preparing Insulin & Giving Injection-Page 2. Intervet.
- ↑ Insulin Therapy-Stability & Storage. RxEd.org.
- ↑ Benson EA, Benson JW Jr, Fredlund PN, Mecklenburg RS, Metz R. (1988). Flocculation & Loss of Potency of Human NPH Insulin. Diabetes Care.
- ↑ Playán J, Acha J, Navarro H, Sanz A, Guallar AM, Albero R. (1994). Flocculation of NPH Insulin. Revista Clinica Espanola-(English Translation).
- ↑ Rosskamp, Ralf H., Park, Glen (1998). Frosting Caused in NPH/Isophane Insulin By Heat/Cold. Journal-Diabetes.org.
- ↑ Definition of Flocculation. Dorlands Medical Dictionary.
- ↑ 35.0 35.1 Diabetes Forecast-Storage & Safety-Frosting of NPH, Lente, Ultralente Insulins-Page 5. American Diabetes Association (2006). Cite error: Invalid
<ref>tag; name "Forecast" defined multiple times with different content - ↑ Humalog and Heat. Diabetesnet.com.
- ↑ Insulin Leaking From Injection Site. Ask the D Team/Children With Diabetes.
- ↑ Griffin, Stacy, Hieronymus, Laura. Insulin Delivery Devices. Diabetes Self Management.
More Information[]
- Diabetes Mellitus Washington State University
Good general information with photos and tips about drawing insulin. - Tips and Tricks from Pet Owners-Alternative to Tent Method Technique PetTalk
Drawing Insulin Pictorial[]
- Drawing Insulin BD Animations
Dogs - Pictorials[]
- Insulin Injections Slideshow BD Pictorial for dogs
- Another one for Dogs Intervet
- Selecting Injection Sites BD Diabetes
Dogs - Online Videos[]
- Dogs Part 1 Intervet
- Dogs Part 2 Intervet
- Cornell University Feline Health Center-Giving Insulin Injections Flash Movie
This contains good general information about drawing insulin and how to give insulin injections--not strictly for cats.
Dogs - Injection Time Tips[]
- Tips on Giving Dogs Shots--Making it less Stressful HealthyPet.com
Injection Site Rotation[]
- Rotating sites BD Diabetes
- Diabetic Skin Disorders

