Iletin from Eli Lilly. Beef R/Neutral in varying strengths--not highly purified, nor were there any suspension insulins at the time. Photo is likely ca. 1922-1923.

Toronto insulin circa 1930.
Insulin is a hormone produced by the beta cells of the pancreas. Insulin delivered into the body through a syringe, insulin pen, pump or other delivery method is known as exogenous insulin--insulin that comes from outside of the body. The role of exogenous insulin in treating diabetes mellitus was first discovered, and the substance refined, in 1921 at the University of Toronto by Sir Frederick Banting, and colleagues Best, Collip, and Mcleod. Commercial production began in 1923 at the newly formed Nordisk Insulin Labs (now Novo Nordisk) in Denmark, and at Eli Lilly and Co. in the USA.
These are the various insulins discussed on this site.
How it works[]
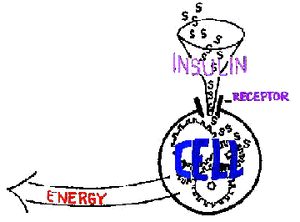
Insulin receptors are cell sites which accept insulin. This allows the cells to accept and use glucose for fuel.
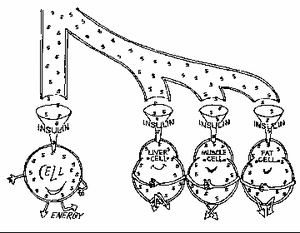
Insulin uses receptors to enter body cells. Glucose can't be used as fuel until it is able to enter the body's cells. Insulin allows glucose to enter body cells, thus the body is able to use the glucose for its fuel.With the insulin system working, insulin allows cells to use glucose found in the bloodstream, keeping them fed and preventing hyperglycemia.
Insulin [1] is necessary to enable the body to perform normally. [2] It controls the rate at which the body's cells can take in fuel (glucose).
Without the insulin system, the body would burn fuel whenever it was available, instead of when it was most needed. It would also burn whatever is available for energy instead of the glucose it's meant to use.
Our bodies normally are "fueled" by burning glucose; they are able to do this provided they have enough insulin (normally or by injection). When there's not enough insulin to allow the body to burn glucose for energy, it begins metabolizing fat to fuel its cells. In particular, the brain cannot go without energy even for a second, so it demands fat conversion to ketones when glucose energy is unavailable. [3] Continuing this process using fat and ketones instead of glucose without sufficient insulin intervention is the path to ketoacidosis.[4]
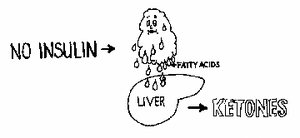
When there's not enough insulin to allow conversion of glucose to energy, the body begins to break down fat cells, which produce fatty acids. These fatty acids are converted to ketones which can fuel the brain in emergencies.
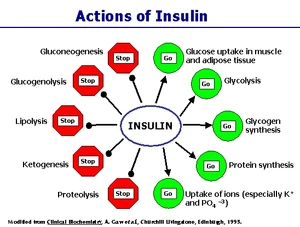
Actions of insulin-the anabolic (positive or energy-producing) bodily process are shown in green--the catabolic (negative or energy-using) ones are in red. [5]
In the cells themselves, insulin aids in the anabolic (a positive, building or maintaining process) processes of turning glycogen, [6] stored in the liver and in muscles, into energy, and helps transform fatty acids and protein into forms both useful and necessary to the body. [5]
It complements or counter-acts the breaking-down the catabolic (breaking-down) [7] body processes of gluconeogenesis, lipolysis, (fat breakdown) and glycogenolysis (glycogen breakdown). [8][9]
In diabetes, insulin is not produced in adequate quantities, or some of the insulin is not accepted by the receptors. While there is plenty of glucose within the system, the body's cells cannot accept it, and suffer what's called intracellular hypoglycemia-the cells cannot get the glucose they need without insulin. [10] The hyperglycemia seen in blood glucose readings represents the glucose present in the body, which, without enough insulin, is unable to use it properly--it's called extracellular hyperglycemia. [11][4]
Insulin secretion[]
Insulin secretion in non-diabetic human. The peaks represent the additional insulin released at meal times, called post-prandial, or after-meal insulin. Here you see how the non-diabetic body automatically calculates how much insulin is needed to handle the extra glucose generated by the meal and releases it.
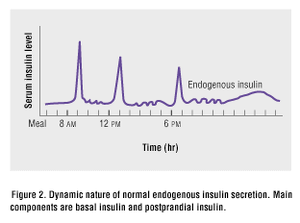
Another view of endogenous (produced by the body) insulin production of a non-diabetic human. The basal, or body's needs minus the processing of food, insulin levels are the lower, often wavy lines shown. The sharp peaks represent how the body responds automatically with secretion of additional insulin to handle the extra glucose creating by eating meals, which are referred to as post-prandial (after-meals) on this graph. People using insulin try to re-create this pattern as much as possible by using fast or short-acting insulin at meal times.
In those without diabetes, the healthy pancreas secretes insulin in pulses or spurts. Basal insulin secretion is a series of small pulses or spurts at a given rate day and night; these insulin pulses or spurts are to take care of the body's basic needs.
When someone without diabetes eats a meal, the pancreas goes into higher gear, turning out larger quantities of post-prandial insulin to handle the additional glucose created by the food. [12] This phase of insulin secretion is often referred to as the first phase, while the steady, slow basal rate is termed the second phase. [13]
Dogs who don't have diabetes have a similar insulin secreting pattern to people who don't have diabetes, with the same two phases intended for the same purposes as in humans. [14]
It is this pattern that diabetics try to mimic as closely as possible; with Basal insulin injections for the body's needs without considering food and Bolus insulin injections to cover meals replacing the Basal and Postprandial insulin their bodies no longer produce or do not produce in sufficient quantity. [15]
The problem in Type 1 diabetes, which dogs have, is that the ability to signal the pancreas to produce insulin is missing; further, the damaged pancreatic beta cells are no longer capable of producing insulin to meet the body's needs for it. If the ability to signal for insulin production could be restored for someone with Type 1 diabetes, there would still be the problem of the pancreas beta cells being unable to supply the needed insulin. This is why insulin injections are necessary to replace the insulin the pancreas can no longer create. Oral medications are only able to help the system either produce more insulin or assist in the ability to use the insulin the pancreas is still able to produce. Those with Type 2 diabetes (which is what most cats have) are able to produce insulin, but the body's cells have lost the ability to use that insulin properly; this is the reason many Type 2 diabetics are able to use oral medications to control the disease. [16][17]
Insulin, then, in 10 words or less, is the hormone that lowers blood glucose and feeds the body. [18] And if you read no further, it would appear that as long as one has some insulin, either endogenous or exogenous, this is simple and everything will be fine.
Kinetics & dynamics[]
When reading various medical literature about insulin and its actions, one often sees the terms kinetics and dynamics used. Knowing what each means in terms of blood glucose can help you understand where it applies to you or your pet.
Insulin Kinetics refers to the time when an insulin can be measured in the bloodstream. It's important to understand that even though it's "officially" made its way there, the insulin has not yet done so in sufficient quantity to effectively begin to lower blood glucose. [19][20]
Insulin Dynamics is the point where it has an effect on blood glucose levels. [21][20][22]
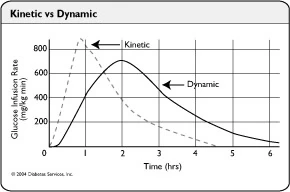
The dotted line shows insulin entering the bloodstream (kinetics).
The bold line (dynamics) illustrates the insulin at the point where
blood glucose is lowered by it.
A good illustration of kinetics and dynamics is having a headache and taking an aspirin for it. You will get relief after the aspirin's level in your system has reached the dynamic stage. While it is in the kinetic one, you are still waiting for headache relief.
Counterpoints to insulin[]
There are other hormones present and also necessary to the body, which do the exact opposite of insulin--raising blood glucose levels. [23] Cortisol, growth hormone, adrenalin AKA epinephrine, glucagon, progesterone [24] and thyroid hormone are considered counterregulatory hormones [25] as far as diabetes and blood glucose levels are concerned.
They need just as much consideration as insulin, because changes in their bloodstream levels can mean a possible interference with insulin, or a need for more of it. These changes can occur normally within the body to supply extra fuel when needed, or as symptoms of a disease state (Acromegaly=too much growth hormone, Cushing's disease =too much cortisol/cortisone, Hyperthyroidism =too much thyroid hormone, Hypothyroidism =too little thyroid hormone, Addison's disease =too little cortisol/cortisone ), or as a result of other medications, such as steroids.
The counter-regulatory hormones such as adrenalin/epinephrine, glucagon and cortisol/cortisone are released to provide extra energy to the body in various circumstances, or if the body believes it's threatened with hypoglycemia. In some cases this is part of the body's "self-defense" mechanism to counter the effects of too much insulin.
So there's more than just insulin one needs to think about. It's vital to life whether enough is produced by the body or whether it's injected. The other hormones are also vital to the body and being able to understand how the various hormones react or interact with each other is very helpful in understanding and successfully controlling diabetes.
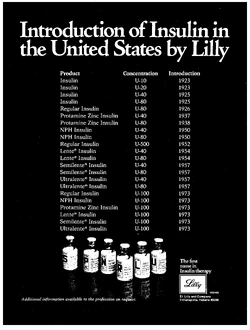
Strength[]
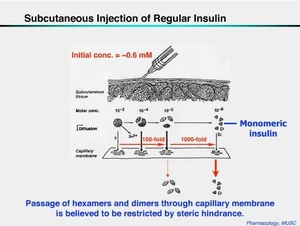
The strength of an insulin is measured in International Units (IUs) of insulin per millilitre (ml). The two most common strengths used in pets are U40 (40 units insulin per ml) and U100 (100 units insulin per ml). U100 insulins are developed primarily for use in humans, although they are commonly used in pets. U40 insulins were commonly available in the US until the 1980's, along with the now-standard U100 strength. They are still available in some countries, but have been phased out in many, in favor of U100. For many years, insulin was produced in varying strengths. [26][27][28][29]
U40 [30] insulins are able to be drawn and dispensed in smaller doses (less than 5 units) with much greater accuracy than their U100 counterparts. This makes them advantageous for use in treating both children and pets, who both have smaller bodies and smaller insulin requirements than adult humans.
U40 insulin has its advantages for more than children and pets.
Less strength=speed[]
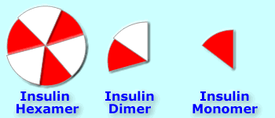
Insulin hexamers must break down into dimers and monomers to be absorbed. [31]
What happens after insulin is injected subcutaneously. It must break down from its hexamer form into dimers and monomers before it can enter the bloodstream via the capillaries to go to work on reducing blood glucose.
The hexamers of insulin tend to associate with each other (stay together) when coming in contact with zinc in the bloodstream; [32] they cannot be readily absorbed while they remain this way. This is also how endogenous insulin is stored in the bodies of those who don't have diabetes--in hexamer form. [33]
Diluting insulin into U40 strength forces them into dissociating (staying apart from each other, and becoming dimers and monomers that can be used by the body), which means they are absorbed [34][35] better and more rapidly. An easy way to visualize this might be to think of a whole pie, slicing it into 6 pieces, then putting each piece on a separate plate. The pie can't be eaten until it's cut and everyone has a piece on his or her plate.
While the body stores insulin in hexamer form, [36] a normally working pancreas secretes insulin in monomer form, so there's no formation of hexamers by self-association and nothing to break down; the monomer insulin is ready to work. [37]
This study compares the absorption rate of U100 and U40 insulins. [38] The findings show U100 insulin to be significantly slower acting than U40 because it has a slower absorption rate. (Note the same study is available through a URL from Diabetes [39] Care--a publication of the American Diabetes Association.) From 30-40 minutes after injection, U40 insulin produces a 20% higher insulin level in the body than the identical amount of U100 insulin injected at the same time. U40 insulin often has a faster onset then does U100 insulin. [31][22]
U40 [40] insulin was also the subject of another 1998 study. This one compared it to both U100 insulin and the rapid-acting analog insulin Lispro, which was the only rapid-acting analog insulin on the market at the time of the study. Insulin lispro, known as Humalog, was found to be only slightly more rapidly absorbed than U40 non-analog insulin. The rapid-acting analog insulins such as Humalog, Novolog, NovoRapid and Apidra have amino acid sequences which are altered to prevent the insulin hexamers from remaining together in self-association. Diluting insulin from U100 strength also prevents this self-association. [41]
The fact that U40 insulin has a similar pharmacokinetic profile to rapid-acting analog insulin, has not been lost on the German Institute for Health Care Quality (government department). They proposed a cost-cutting move which would limit prescription coverage of the rapid-acting analogs in Germany. [42]
More strength=duration[]

Humulin R U 500 strength. Note that the vial is 20 ml--twice the size of the standard 10 ml ones and the striping on the carton to alert users to the fact that this insulin is 5 times the strength of standard U 100 insulins. [43]
1975 JAMA ad for Lilly insulins detailing history. U 500 was marketed in 1952; U 100 insulins not until 1973.
It is also possible to delay the absorption of an insulin by increasing the strength of its concentration. [22] U500 insulin, [44] which is five times more concentrated than U100, has been available through both Lilly and Novo Nordisk (Note: Their similar product is U400 strength insulin [45]) by special order for many years. [46] The insulin's main use is for people with extreme Insulin resistance, and is commercially available only in R/Neutral type.
Though it is R/Neutral-type insulin, U400 & U500 insulins [47] have a pharmacokinetic profile more like NPH insulin than U100 R/Neutral. [48][43]
Since there are no additives such as suspensions to alter R/Neutral insulin's action, the strength of the insulin formula hinders its breakdown into dimers and monomers, thus making it much slower-absorbed than U100 and lesser strength insulins. [49][50][51]
In cases of severe insulin resistance, using a much higher concentration of insulin appears to "negate" the effects of immune-related insulin resistance.
The studies at the link below shows that there was no difference regarding antibodies when these patients were transferred from Iletin II NPH at U100 strength to a form of Iletin II R at U500 strength. However, the stronger insulin reduced their insulin needs from 33-75%. [52][53]
Types by length of action[]
Insulins are categorized first by length of action, then by origin and by suspension. The four durations are: [54]
| Insulin types: length of action | |
|---|---|
| Rapid onset-fast-acting (analog) insulin | |
| Short-acting insulin | |
| Intermediate-acting insulin | |
| Long-acting insulin |
The usual times for onset, peak, and duration are found with the information for the insulin itself, but they also depend on the species, the suspension, and the individual. So the times found here [55] are average for humans and dogs.
This insulin chart [56] is a bit dated, but seems to be a good guide to onset, maximum effect (peak) and duration.
Types by origin[]
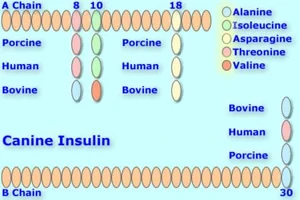
Canine insulin compared to Bovine, Porcine, and Human versions. Up to 2 amino acids differ with canine and porcine being identical. [57]
Porcine insulin is identical to canine. Bovine insulin is similar to feline, [58] differing by only a single amino acid in position 18. (Mnemonic device: piG = doG, Cow = Cat). Both differ in up to four amino acids (positions 8, 10, 18, 30) from natural human insulin. [59] Porcine (pig) and bovine (cow) insulins can be combined to produce a "blended" insulin (such as Iletin I (beef/pork) and PZI Vet). Genetically-engineered artificial insulins with different amino acid composition such as Lantus, Levemir, Humalog, Novolog, and Apidra, are known as analog insulins.
Origin, species, or source is very important as it directly affects the absorption, peak and duration of an insulin. [60][22]
Insulins differ by species. Most commonly available types are:
| Insulin-types: species/origin | |
|---|---|
| r-DNA human insulin Genetically-engineered (GE) human insulin Genetically-modified (GM) human insulin | |
| porcine (pork) insulin | |
| bovine (cow) insulin | |
| human analog insulins |
| Amino Acid Sequence of Insulin Preparations [61] | |||||||
|---|---|---|---|---|---|---|---|
| Amino Acid Substitutions | |||||||
| A-Chain Position | B-Chain Position | ||||||
| Source Species |
A-8 | A-10 | A-21 | B-28 | B-29 | B-30 | B-31 B-32 |
| Beef | Ala | Val | Asn | Pro | Lys | Ala | N/A |
| Pork | Thr | Ilc | Asn | Pro | Lys | Ala | N/A |
| Human | Thr | Ilc | Asn | Pro | Lys | Thr | N/A |
| Aspart | Thr | Ilc | Asn | Aspartic Acid | Lys | Thr | N/A |
| Lispro | Thr | Ilc | Asn | Lys | Pro | Thr | N/A |
| Glulisine | Thr | Ilc | Asn | Pro | Glu | Thr | N/A |
| Lantus (glargine) | Thr | Ilc | Gly | Pro | Lys | Thr | Arg |
| Levemir(detemir) | Thr | Ilc | Asn | Pro | Lys | N/A | Myristic Acid |
|
| |||||||
Types by suspension[]
| Insulin types: suspension | |
|---|---|
| Clear soluble insulins have no suspension. | |
| Isophane (protamine) suspension | |
| Protamine Zinc suspension | |
| Zinc suspension |
The suspension (liquid the insulin is suspended in) is the key to its activity over time. Typical suspensions are Isophane: (NPH, Mixed), Zinc: (Lente, semilente, Ultralente) and Protamine Zinc: (PZI). In general, all insulins with the same suspension will have a similar time activity profile and behave similarly. In non-analog insulins, it is the suspension that makes intermediate and long-acting types work longer than R/neutral.
|
Manufactured insulin diluents contain both suspension and preservative additives which are also present in the insulin(s) they are made to dilute. Using the wrong diluent for an insulin may alter its activity profile, causing the insulin to work to rapidly or too slowly. This is one reason why insulins should be diluted only with the correct approved diluent for that insulin. [62] | ||
Guidance on use[]
Before each use, take a moment to inspect the insulin prior to drawing it into the syringe; clear insulins should appear not discolored and clear; suspended insulins should be uniform in their cloudiness. [63]
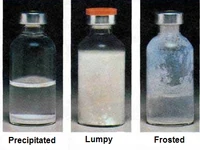
Three visual examples of damaged insulin.
|
Do not use the insulin if:
See Insulin problems for more information about "bad" insulin. | ||
If you made a mistake and forgot to put the insulin back into the refrigerator, even for several hours, there should be no problem. Many keep their insulin (see instructions for your brand) at room temperature all the time. [72] When comparing it to insulin which is in the fridge except when used, it may be more likely to have slight potency loss. When a vial has been left out of the refrigerator for some time, it needs to be monitored for any signs of frosting; [73] in the photo, the vial on the right is an example of frosting. If the insulin was exposed to heat or direct light for a while when it was out of the refrigerator, or shaken vigorously or dropped a long way, the best thing to do would be to start with a new vial. [74] ![]()
See injecting insulin, resuspending insulin, drawing insulin, diluting insulin, combining insulin, combining insulin tutorial and insulin use tips.
For dosage see regulation and insulin starting doses.
For syringe information see syringe and syringe parts.
Note that any insulin, given in overdose, can lead to hypoglycemia and coma or death. See avoiding hypos.
For basic insulin use terms, see Onset, Peak, Nadir and Duration.
For advanced use see also basal, bolus, and corrective insulin.
For what can go wrong with insulin see absorption, and regulation difficulties, especially the Insulin problems section.
References[]
- ↑ Nussey, S.S., Whitehead, S.A. (2001). Endocrinology, an Integrated Apporach-Insulin. National Institutes of Health.
- ↑ Grooters, Amy M., (April 1999). Insulin is essential for many metabolic processes. ACVIM.
- ↑ Energy Metabolism Explained.
- ↑ 4.0 4.1 Tabor, Kim (February 2011). Diabetic Ketoacidosis. Veterinary Technician.
- ↑ 5.0 5.1 Dean, Laura. The Genetic Landscape of Diabetes. National Institutes of Health.
- ↑ Glycogen Description/Definition. Dorlands Medical Dictionary.
- ↑ Catabolic Definition. Dorlands Medical Dictionary.
- ↑ Glycogen Breakdown Explanation. Dorlands Medical Dictionary.
- ↑ Physiological Functions of Insulin. Pediatric Oncall.
- ↑ Pathogenesis-Diabetes Mellitus. Intervet.
- ↑ Diagram-Pathophysiology of Diabetes Mellitus-Insufficient Insulin--What Happens. Intervet.
- ↑ Illustration of how much of the secreted insulin is basal (body needs) and how much is prandial (meal) insulin in a non-diabetic. Pediatric Oncall. Archived from the original on 2013-06-24.
- ↑ Insulin Release. Wikipedia.
- ↑ Hess, Rebecka S. (May 2008). Managing Diabetes Mellitus in Dogs. DVM 360.
- ↑ White, John R., et. al. (June 2003). Novel insulins and strict glycemic control. Postgraduate Medicine.
- ↑ Better Medicine-E-Newsletter. Intervet (June 2006).
- ↑ Schall, William (2009). Diabetes Mellitus-CVC Proceedings-Drugs other than insulin and insulin analogs used to treat diabetic human beings. DVM 360.
- ↑ Diagram of Insulin's Effects on the Body. Intervet.
- ↑ Fischer U, Freyse EJ, Jutzi E, Besch W, Raschke M, Höfer S, Albrecht G. (1983). Absorption rates of subcutaneously injected insulin in the dog as calculated from the plasma insulin levels. Diabetologia.
- ↑ 20.0 20.1 Pharmacokinetics vs Pharmacodynamics. Endotext.org.
- ↑ Insulin Kinetics & Dynamics. Diabetesnet.com.
- ↑ 22.0 22.1 22.2 22.3 Heinemann, Lutz (January 2008). Variability of Insulin Action:Does It Matter?. Insulin Journal.
- ↑ Carbohydrate Hormone Control. Elmhurst College.
- ↑ Brooks, Wendy C.. Explanation of Progesterone's Functions. Veterinary Partner.
- ↑ Counter-Regulatory Hormones. rnceus.com.
- ↑ Insulin by Connaught 10 units 5 c.c. vial-10 units per c.c. 1923. University of Toronto.
- ↑ Lilly Iletin--1922--20 units in 5 cc. University of Toronto.
- ↑ Iletin Vial and 2 Cartons-1923. Carton on Right is U20-U40 Carton is on Left.
- ↑ Closer Look at Iletin 1923 Vial.
- ↑ Accuracy of Dosing U40 Insulin. British Medical Journal-Register Free to View.
- ↑ 31.0 31.1 Hanas, Ragnar (1999). Insulin Dependent Diabetes-page 5. Children With Diabetes.
- ↑ Insulin. Islets of Hope.
- ↑ Insulin. Wikipedia.
- ↑ Sindelka G, Heinemann L, Berger M, Frenck W, Chantelau E. (1994). Effect of insulin concentration, subcutaneous fat thickness and skin temperature on subcutaneous insulin absorption in healthy subjects. Diabetologica.
- ↑ Hirsch, Irl (1999). Type 1 Diabetes Mellitus & Use of Flexible Insulin Regimens. American Family Physician.
- ↑ Insulin. Wikipedia.
- ↑ Abrams-Ogg, Anthony (2007). Chemistry and Pharmacology of Therapeutic Insulin Preparations. ACVIM.
- ↑ Hildebrandt P, Sestoft L, Nielsen SL. (1983). The absorption of subcutaneously injected short-acting soluble insulin: influence of injection technique and concentration. Diabetes Care.
- ↑ Copy of Reference above in ADA's Diabetes Care Publication.
- ↑ Polaschegg E. (1998). Effect of physicochemical variables of regular insulin formulations on their absorption from the subcutaneous tissue. Diabetes Research and Clinical Practice.
- ↑ Hildebrandt P. (1991). Subcutaneous Absorption of Insulin in Insulin-Dependent Diabetic Patients. Influence of Species, Physico-chemical Properties of Insulin and Physiological Factors. Danish Medical Bulletin.
- ↑ Rapid-acting insulin analogues in diabetes mellitus type 1: Superiority not proven. IQWiG-German Institute for Quality and Efficiency in Health Care (6 June 2007).
- ↑ 43.0 43.1 Cochran, Elaine (2009). U-500 Insulin. Diabetes Spectrum.
- ↑ Resource Guide. American Diabetes Association (2005).
- ↑ Cochran, Elaine, et. al. (2005). of U500 Insulin in Patients With Extreme Insulin Resistance. -Diabetes Care.
- ↑ Diabetes Forecast-page 4. American Diabetes Association (2006).
- ↑ Quick, Bill (September 2008). Dr. Bill's Blog. Diabetes Monitor.
- ↑ Questions About Insulin. Diabetes-World Mailing List.
- ↑ Jørgensen KH, Hansen AK, Buschard K. (2000). Five Fold Increase of Insulin Concentration Delays the Absorption of Human Insulin Injections in Pigs. Diabetes Research & Clinical Practice.
- ↑ Lane WS. (2006). Use of U500 R Insulin by Continuous Insulin Infusion (Insulin Pump)in Patients With Type 2 Diabetes & Severe Insulin Resistance. Endocrine Practice.
- ↑ Humulin R-U500 Patient Leaflet. Eli Lilly.
- ↑ Nathan DM, Axelrod L, Flier JS, Carr DB. (1981). U500 Insulin in the Treatment of Antibody-Mediated Insulin Resistance. Annals of Internal Medicine.
- ↑ Baumann G, Drobny EC. (1984). Enhanced Efficacy of U500 Insulin in the Treatment of Insulin Resistance Caused by Target Tissue Insensitivity. American Journal of Medicine-1984.
- ↑ Insulin Therapy. RxEd.org.
- ↑ Insulin Activity Profiles. HealthLine.
- ↑ Newman, Chick. Time Activity Profiles Insulin Chart--Dogs and Cats. Newman Veterinary.
- ↑ Caninsulin-Product Information. Intervet.
- ↑ Feline Insulin Sequence. Science Direct.
- ↑ Insulin Amino Acid Sequences. Petdiabetes.org.
- ↑ Diabetes Forecast-page 3. American Diabetes Association (2006).
- ↑ Guide to Insulin Preparations. Phamacy Times.
- ↑ Lilly Discontinues Diluent for all Lente & Ultralente Insulins. Eli Lilly.
- ↑ Insulin Therapy-Stability & Storage. RxEd.org.
- ↑ Benson EA, Benson JW Jr, Fredlund PN, Mecklenburg RS, Metz R. (1988). Flocculation & Loss of Potency of Human NPH Insulin. Diabetes Care.
- ↑ Playán J, Acha J, Navarro H, Sanz A, Guallar AM, Albero R. (1994). Flocculation of NPH Insulin. Revista Clinica Espanola-(English Translation).
- ↑ Rosskamp, Ralf H. Park, Glen (1998). Long Acting Analog Insulins-Frosting Caused in NPH/Isophane Insulin By Heat/Cold. Journal-Diabetes.org.
- ↑ Patchuki, Linda, et. al. (1 November 1987). Flocculation of Insulin Preparations. Annals of Internal Medicine.
- ↑ Definition of Flocculation. Dorlands Medical Dictionary.
- ↑ 69.0 69.1 Diabetes Forecast-Storage & Safety-Frosting of NPH, Lente, Ultralente Insulins-Page 5. American Diabetes Association (2006).
- ↑ Humalog & Heat. Diabetesnet.com.
- ↑ Injecting Insulin-Transcript of American Diabetes Association Videotape. American Diabetes Association (2003).
- ↑ Travelling With Insulin. FAQs.org.
- ↑ Insulin Update-storage of insulin. Nora Apothecary.
- ↑ Tips on Caring for Diabetic Pets. Diabetic-help.com.
More Information[]
- Diabetes control in Siberian Husky Richards, Mike, Vet Info.com
Case details about using R/neutral and/or mixed insulins in dogs. - More details on insulin types for animal use Elephantcare.org
- More general insulin information Endotext.org
Good illustrations and charts for seeing where bovine and porcine insulins differ from human insulin and how analog insulins Lantus (insulin glargine), Novolog (insulin aspart), and Humalog (insulin lispro) have been altered to produce their respective effects. Some absorption discussion related to humans, some of which is relevant to animals, as absorption is an important factor in how the insulin is used for all with diabetes. Time activity profiles for everything except Levemir and any PZI. Aspart/Lispro chart would be applicable for the new Aventis Apidra, as it is also a rapid-acting insulin designed for bolus in humans. - The History of Insulin
- The Discovery of Insulin
- The Discovery and EarlyDevelopment of Insulin University of Toronto
- All About Insulin In Depth In Chem
- Time Activity Profile Tables for human approved insulins sold outside of North America
- A chart of the variations in amino acid sequence on the A and B chains of different species Diabetes in Pets.
- Dr. Ragnar Hanas
is a Swedish pediatrician whose book about Insulin-Dependent Diabetes is clearly written and easy to understand. Unlike many doctors, you feel she's talking with you and not down to you. Even though it was written in 1999 and insulins Lantus and Levemir were not yet marketed, the explanations are classic. She intended it for explaining human diabetes, but there is much we can gain from it too. The link is to a chapter she graciously donated to Children With Diabetes. - Click Here To View Time Activity Profiles of Lilly Insulins in humans and dogs
- Insulin Comparison Chart--All But Levemir & Apidra HealthCanada
- Intro to Diabetes and Insulin HealthCanada
- Insulin Synthesis & Secretion CSU Veterinary School of Medicine
- Physiologic Effects of Insulin CSU Veterinary School of Medicine
- Physiological Effects of Insulin Rnceus.com
- NetDoctor.co.UK List of Insulins in the UK
- Type I Diabetes and Insulin Therapy Hirsch, I, Farkas-Hirsch, A., 1993, Nursing Clinics of North America
- Selecting an Insulin for Treatment of Diabetes Mellitus in Dogs & Cats-page 39 Nelson, Richard, 2006, OSU Endocrinology Symposium
- Switching to Another Insulin: What & How North American Veterinary Conference 2006
- Evaluating Insulins for Companion Animals Abrams-Ogg, Anthony, 2007, ACVIM
- Hormones Which Raise or Lower Blood Glucose Clinical Chemistry
- Insulin and Glucagon Tutorial and Animation
- NACDS-Insulin Chart-Page 2
- Variability of Insulin Action-Does it Matter Heinemann, Lutz, 2008, Insulin Journal
- Successful intensive insulin treatment of type 1 diabetic dogs leads to restoration of peripheral leukocyte insulin signaling gene expression and enzyme activities Mori A, Lee P, Sako T, Mizutani H, Arai T., 2009, Journal of Veterinary Medical Science
- Lente Insulins-Injectable Suspensions West Virginia University College of Pharmacy-2009